Patient-Centric Communication for the Omnichannel Future
Patient Relationship Management: Understanding the full context of the patient in an increasingly complex healthcare system
Disclosure: This research brief was produced with support from Innovaccer given our shared interests in educating users about the importance of effective PRM, which we have been writing about for years now. You can be confident that even when producing sponsored content, our objectivity in presenting the materials is fundamental to our credibility and mission, so these are developed to be educational, never promotional.
The COVID-19 pandemic made it clear how essential communication with patients outside of clinical encounters is. Unfortunately, with limited tools and staff, patient outreach often suffered. Consumer Relationship Management (CRM) platforms offer tools and workflows to address some of those problems, but their design and focus on a sales-oriented transactional engagement model often does not match up with the full breadth of needs in healthcare. Patient Relationship Management (PRM) platforms pair the functionality and tools of a CRM platform with a clinically and financially integrated patient-centric design that offers essential functionalities for evolving care and reimbursement models of healthcare.
This research brief provides ideas and insights for healthcare organizations seeking to understand the differences between Consumer Relationship Management and Patient Relationship Management. It can assist with the identification of organizational needs and digital transformation efforts. As organizations look to select and work with relationship management vendors, they can apply what they learn here when defining reasonable expectations, identifying necessary components, and selecting the correct platform for their goals.
Key Takeaways:
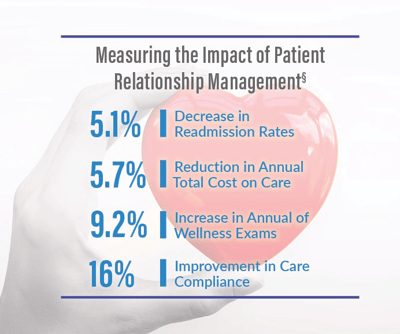
- Patient communication and engagement can have a significant impact on health outcomes, especially in longitudinal chronic care.
- Relationship Management platforms need to be designed to understand and address the full context of a patient. Communication, education, and outreach all need to be tailored to specific patient circumstances and needs to have meaningful effects on patient loyalty and health.
- As patient healthcare expands to include more providers, applications, and devices, a Relationship Management platform needs to integrate and act on data from as many sources as possible. This can include clinical, non-clinical, payer, employer, consumer, and SDoH data.
- The impact on healthcare outcomes makes a Relationship Management platform an essential healthcare tool, regardless of reimbursement or revenue model.
For more market perspectives from our team, take a look at some of the related content below:
- Virtual Care Management: Solutions Enabling Omnichannel Care
Market Trends Report from Alex Lennox-Miller| Virtual care plays an essential role in solving the problems of modern healthcare. The necessary remote appointments and home care of the COVID pandemic have driven use of virtual care to new heights, but its real promise goes far beyond these uses. When seen as part of a system of distributed healthcare, virtual care can play a vital role in the long-term care relationships that occupy most of the modern healthcare system. Learn more about this research here. - 2018 Patient Relationship Management Market Scan Report - Free
Report from Brian Eastwood | This Market Scan Report examines the market forces driving health care organization (HCO) interest in solutions that promise more targeted patient outreach, coordinated care management, and greater opportunity for patient self-management between care episodes. - SDoH, Data Standards, and Innovation for Unstructured SDoH Data
Post from Jody Ranck | A fundamental component of making SDoH strategies more effective rests on the development and use of standards for SDoH data that can facilitate data computability and sharing. Recent efforts by the ONC on the standards front, as well as some innovative approaches utilizing NLP to unlock value from unstructured data in EHRs relevant to SDoH interventions, are on the horizon.
